A 61 year-old female patient suffers from 2 tumors of her right breast which are abandoned for 2 years by a deadly illness of her husband.
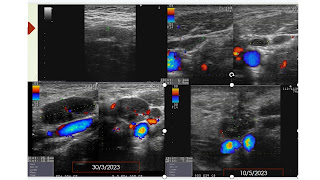
Ultrasound and elastography technique represent two BI-RADS 4B tumors of her right breast which one has perivascular signals.
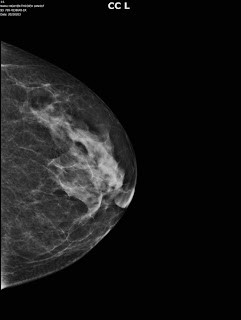
Mammography notes an asymetric sign in superiolateral region of the right breast.
MRI confirms the two BI-RADS 5 right malignant breast tumors: # 34x28 mm and # 21x 27 mm, with spiculated border, high signals on T2W2 and moderate signals on T1W1, captured contrast media type 3.
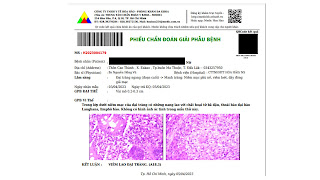
But the report of histoimmunology of the breast tumor is a breast sarcoma while axillary lymph nodes are not in malignancy.
Surgery is done in large field, no mastectomy nor lymph node curetage due to the sarcoma tumor characters.
As no clue of gene mutation, the patient goes through a planning of radiation therapy for 3 months of 54 Gy dosages in 27 times.
A rare case report of breast sarcoma - PMC-NCBI.
Primary breast sarcoma: case report-African Journal online.
Breast sarcoma: a case report and review of literature.















.jpg)
.jpg)
.jpg)
.jpg)










