Man 38yo 2 years ago intermittent hematuria, today
acute right renal colicky pain.
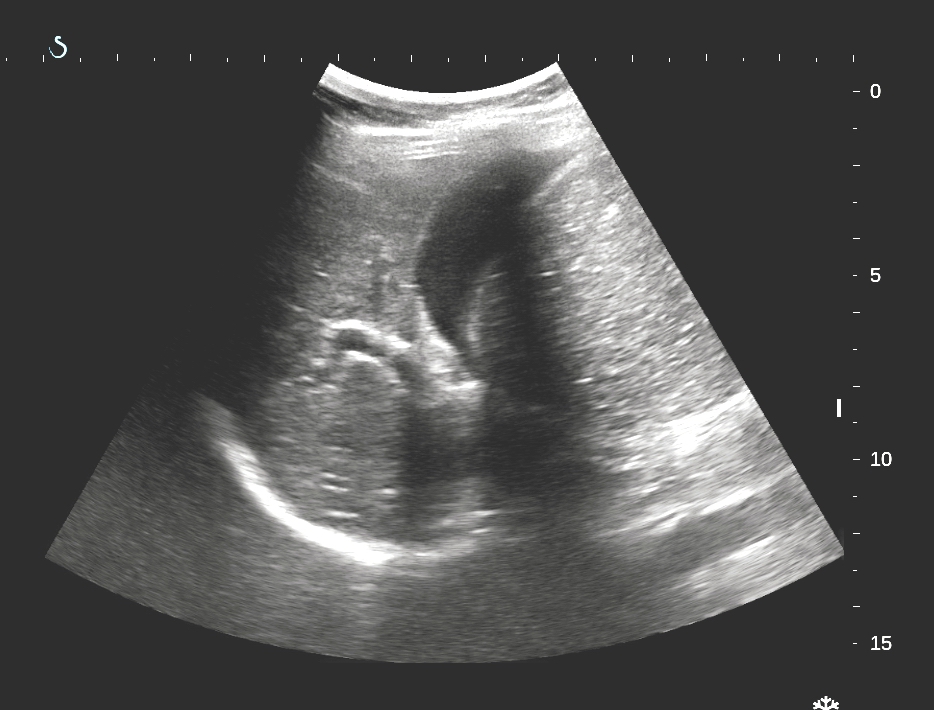
Ultrasound in emergency detected big right kidney and fluid
collection arround kidney.
Pelvic kidney has a collected hyperechoic mass which made dilated ureter.
CDI ultrasound detected no Doppler signal in vascular renal cortex ( US 2)
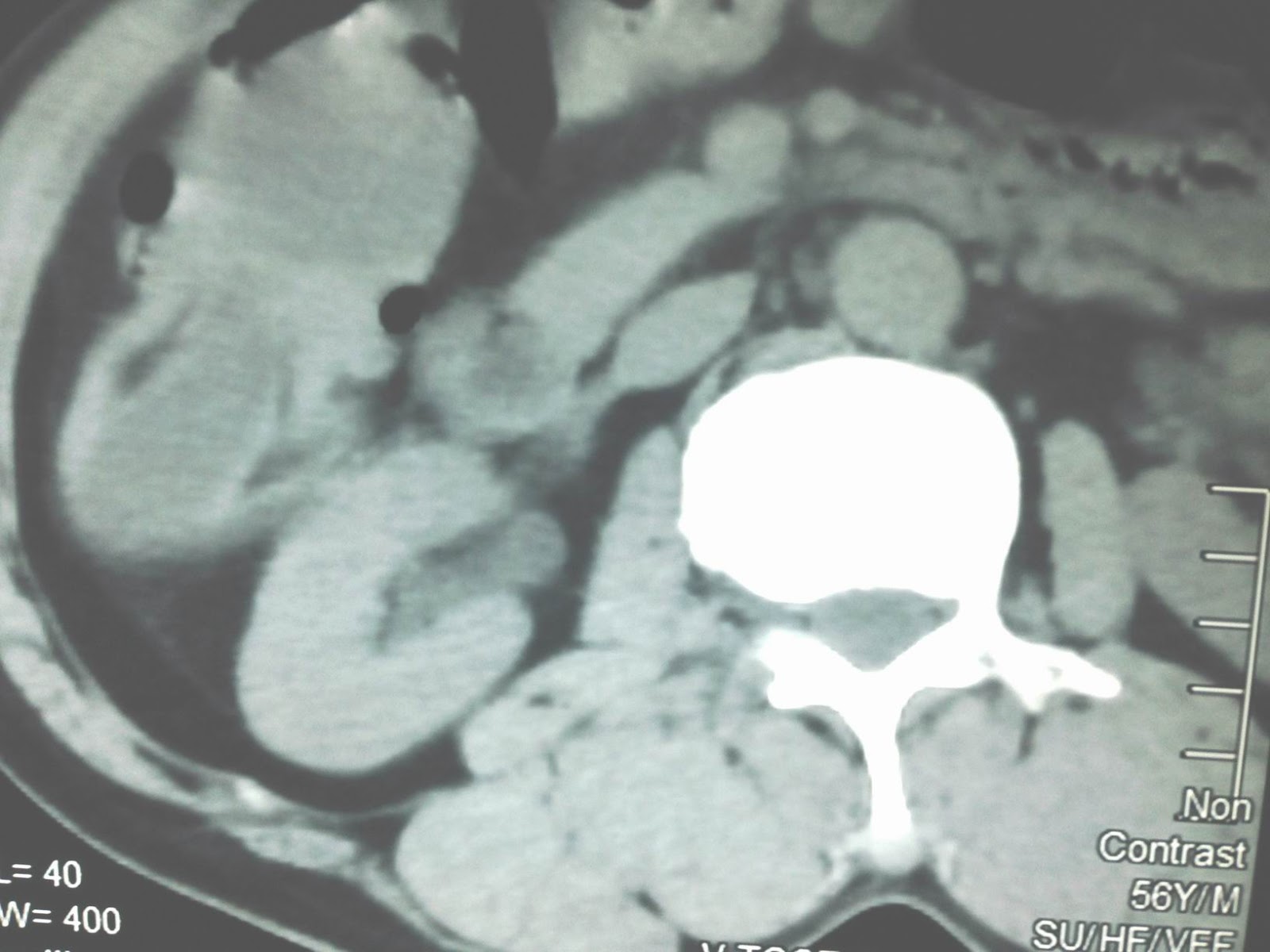
MSCT with CE=CT1: frontal
view= right kidney too big without contrast supplying.
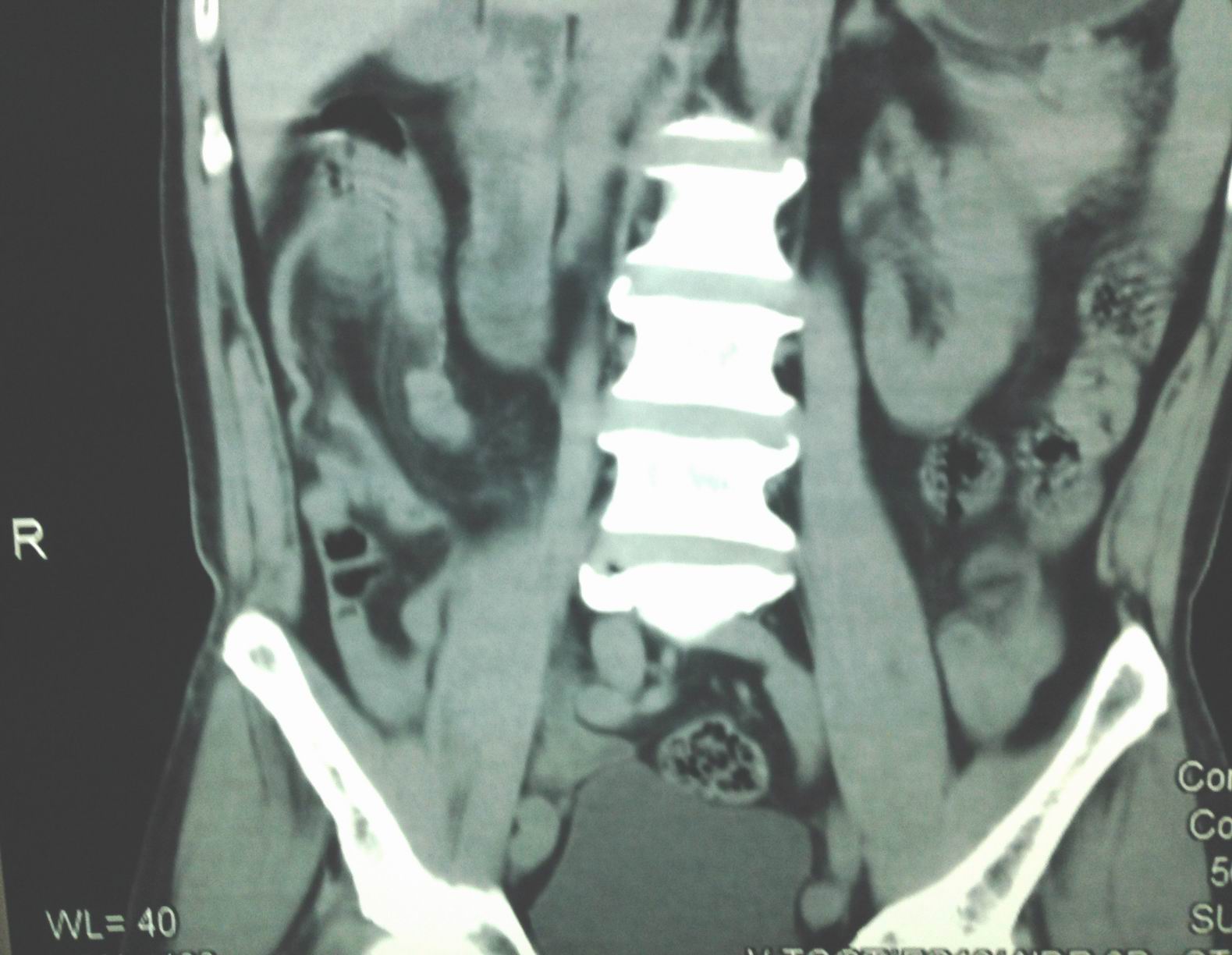
CT 2: frontal view, pelvis of right kidney is covered by enhanced contrast mass just to dilated ureter.
CT3, CT 4: cross- sectional view: pelvis and ureter detected
intralumen one enhanced contrast structure liked a tumor.
CT 6: 3D vascular view= no vascular supplying to right kidney.
Report by radiologist is bleeding intra right urinary system with ureter obstruction by tumor, suspected TCC.(TRANSITIONAL CELL CARCINOMA)
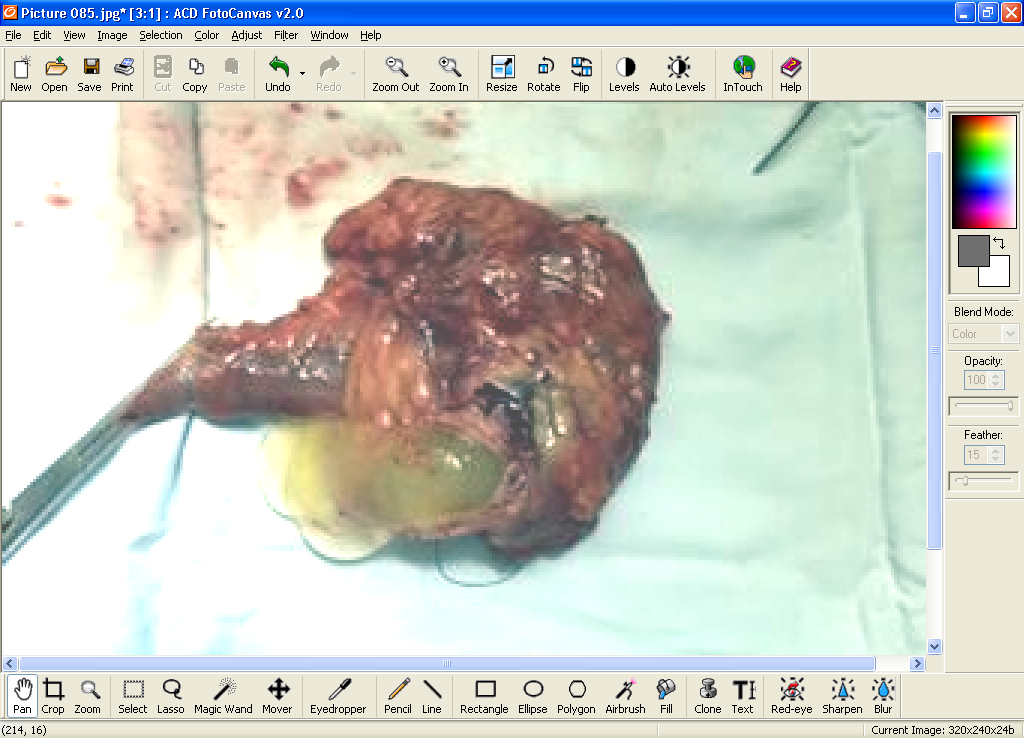
Emergency operation of right nephrectomy and ureterectomy.
Macroscopic specimen showed tumor in obstruction of distal ureter.