case-336-leg-abscess-for-2-years-due-to-missed-foreign-body-
Total Pageviews
Sunday 27 September 2015
CASE 336:02 year Abscess in Leg Muscle due to Missed Foreign Body, Dr LÊ THANH LIÊM, Dr LÊ THÔNG LƯU, Dr PHAN THANH HẢI, MEDIC MEDICAL CENTER, HCMC, VIETNAM
FOR PICTURES PLS CONNECT TO 3 G / DOWNLOAD THE LINK
case-336-leg-abscess-for-2-years-due-to-missed-foreign-body-
case-336-leg-abscess-for-2-years-due-to-missed-foreign-body-
Thursday 24 September 2015
CASE 335: HEMOPERITONEUM, Dr PHAN THANH HẢI, MEDIC MEDICAL CENTER, HCMC, VIETNAM.
FOR PICTURES PLS CONNECT TO 3 G / DOWNLOAD THE LINK
WOMAN 33 YO, ACUTE
LEFT PELVIC PAIN, ULTRASOUND EMERGENCY SHOWED NORMAL
SIZE OF UTERUS, ENDOMETRIUM IN MIDDLE OF MENSTRUAL CYCLE, AND HAVING A
LOT OF FLUID AND BLOOD ARROUND UTERUS TO MORRISSON'S SPACE OF ABDOMEN.
IT WAS A CASE OF HEMOPERITONEUM.
ULTRASOUND
DETECTED ONE ROUND MASS AT LEFT PELVIS WHICH WAS SUSPECTED AN OVARY CYST WITH SIZE OF 4
CM.
PUNCTION OF ABDOMEN AT RIGHT ILIAC FOSSA REMOVED OLD
BLOOD.
BLOOD TESTS WERE NORMAL BETA HCG, Hct 21%, NORMAL AMYLASEMIA.
MSCT WITH CE DETECTED 2 MASSES BOTH 2 SIDES RIGHT
AND LEFT UTERUS; THE LEFT ONE WAS
VERY QUICK CE ENHANCED IN COMPARISON TO THE RIGHT ONE
NON-CE ENHANCE.
Patient was in admission of emergency of surgery hospital.
After receiving of 2 units of blood transfusion, the vital status was stable.
Follow- up by ultrasound one week later the blood clot in pelvis was not rising but not dissolved. Laparoscopic surgery for washer this blood and detected right ovary was normal, while left ovary had ruptured one cyst but already stop bleeding.
Report of surgeon was rupture of luteinic corpus with blood loss more than 2,000 ml-- a severe case of internal bleeding.
After receiving of 2 units of blood transfusion, the vital status was stable.
Follow- up by ultrasound one week later the blood clot in pelvis was not rising but not dissolved. Laparoscopic surgery for washer this blood and detected right ovary was normal, while left ovary had ruptured one cyst but already stop bleeding.
Report of surgeon was rupture of luteinic corpus with blood loss more than 2,000 ml-- a severe case of internal bleeding.
Friday 18 September 2015
CASE 334: MULTIPLE HEPATIC TUMORS: Dr PHAN THANH HẢI, MEDIC MEDICAL CENTER, HCMC, VIETNAM.
FOR PICTURES PLS CONNECT TO 3G / DOWNLOAD THE LINK
case-334-multiple-hepatic-tumors-
case-334-multiple-hepatic-tumors-
WOMAN 43YO, CHRONIC INFECTED HBV, PAIN AT LIVER.
ULTRASOUND DETECTED INTRA HEPATIC MULTIPLE
FOCAL LESIONS WITH SUGGESTION OF LIVER HEMANGIOMA (US1, US 2).
REPORT OF MSCT WITH CE WAS MADE
DIAGNOSIS OF MULTIPLE FOCAL HCC ( CT 1, CT 2).
MRI WITH PRIMOVIST ALSO WAS DIFFUSE
HCC.
BLOOD TEST OF WAKO WERE NEGATIVE, CEA AND CA 19-9 WERE IN NORMAL LEVEL.
FIBROTEST WAS SCORED F2.
DISCUSSION: History were chronic infected HBV and Wako triple test negative. Do you trust in reports of ultrasound, CT with CE, and MRI Primovist ?
Biopsy report is adenocarcinoma metastasis from GI tract.
It is a case of CUP (cancer unknown primary).
Monday 14 September 2015
CASE 333: LUNG MASS, Dr PHAN THANH HẢI, MEDIC MEDICAL CENTER, HCMC, VIETNAM
FOR PICTURES PLS CONNECT TO 3G / DOWNLOAD THE LINK
Man 52 yo, fever
unknown origine for 3 months, blood
tests: nothing abnormal detected.
MSCT
scan of full body detected a small
nodule on right lung, size of
1 cm with some pericarena lymph nodes
enhanced with CE and one subcutaneous
mass of 3 cm in the back of left neck (CT
lung images).
Ultrasound
of this mass revealed round
border, very hypoechoic, nonvascular
filling intramass, no posterior enhancement, no sister mass together ( see 3 US
images and video clip).
Biopsy was done for this
mass and microscopy result was
adenocarcinoma metastasis from the lung.
Discussion: Clinical onset is fever unknown origine, CT lung detected small spicular nodule , pericarena nodes and the patient himself detected one subcutaneous mass at posterior of his left neck; biopsy of this mass made diagnosis of metastasis from lung cancer which is small cell lung cancer.
Conclusion = Small lung cancer metastasis to skin and
paraneoplasic fever.
Reference: Case in NEJM.Friday 11 September 2015
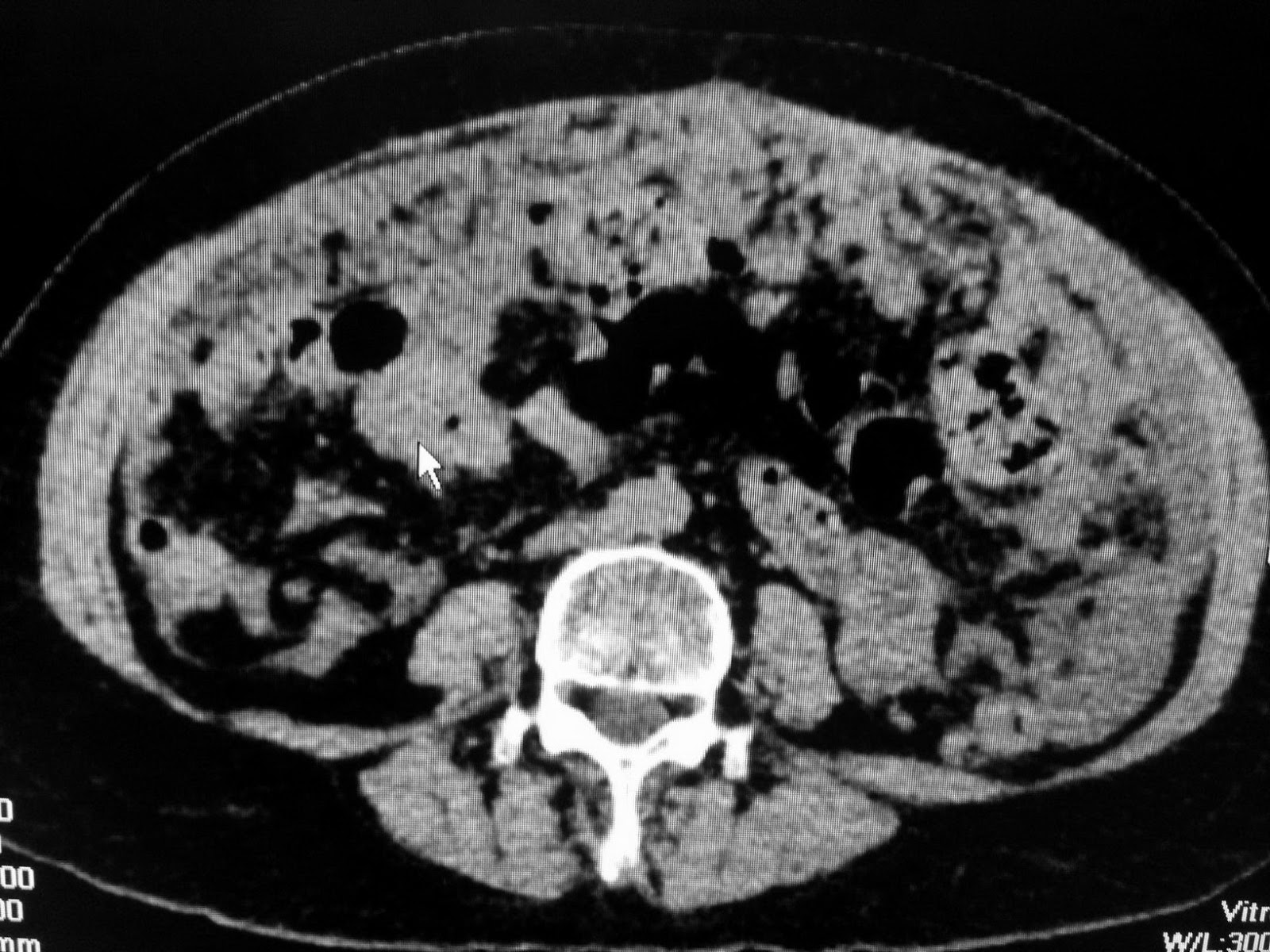
CASE 332 : PERITONEAL CARCINOMATOSIS, Dr PHAN THANH HẢI, MEDIC MEDICAL CENTER, HCMC, VIETNAM.
Woman 68 yo with abdomen distension and pain.
Ultrasound scan detected ascites with pelvic mass ( US images) suspected
peritoneal carcinomatosis.
CT scan of abdomen with CE with radiologist
report was peritoneal carcinomatosis,
unknown primary cancer (CUP).
Blood tests: raised CEA and CA-125 markers.
Abdomen tap removed gelatineous fluid that analysis of this fluid no
cancer cell revealed.
Laparoscopy biopsy of peritoneal vegetation reported mucinous carcinoma.
Discussion: In this case of 68 yo female ascites like jelly, CT and ultrasound cannot detected ovary tumor. Blood tests pointed CEA very high in comparison to CA-125. The most common cause is from rupture of appendiceal.carcinoma and spreading intraperitoneum.
Monday 31 August 2015
CASE 331: MASS INSIDE STOMACH, Dr PHAN THANH HẢI, MEDIC MEDICAL CENTER, HCMC, VIETNAM.
FOR PICTURES PLS CONNECT 3G / DOWNLOAD THE LINK
Child 5 yo long history of epigastric
pain and anorexia treated as HP
infected gastritis.
Ultrasound detected intragastric
mass with large UMBRELLA SIGN [showdown like the
sunshine over the umbrella] which covered more 50% of lumen of stomach ( see US pictures 1, 2, 3).
MSCT of abdomen revealed this
mass inside stomach, multilayer structure, not developmental from the wall of stomach.
Based on ultrasound and abdomen CT, suggestion of radiologist is gastric trichobezoar.
What is your suggestion,
endoscopy or operation for removing the mass inside stomach?
Operation of gastrostomy removed the hair mass.
Reference:
Umbrella's sign of ultrasound.
https://www.google.com/?gfe_
Operation of gastrostomy removed the hair mass.
Reference:
Umbrella's sign of ultrasound.
https://www.google.com/?gfe_
Saturday 15 August 2015
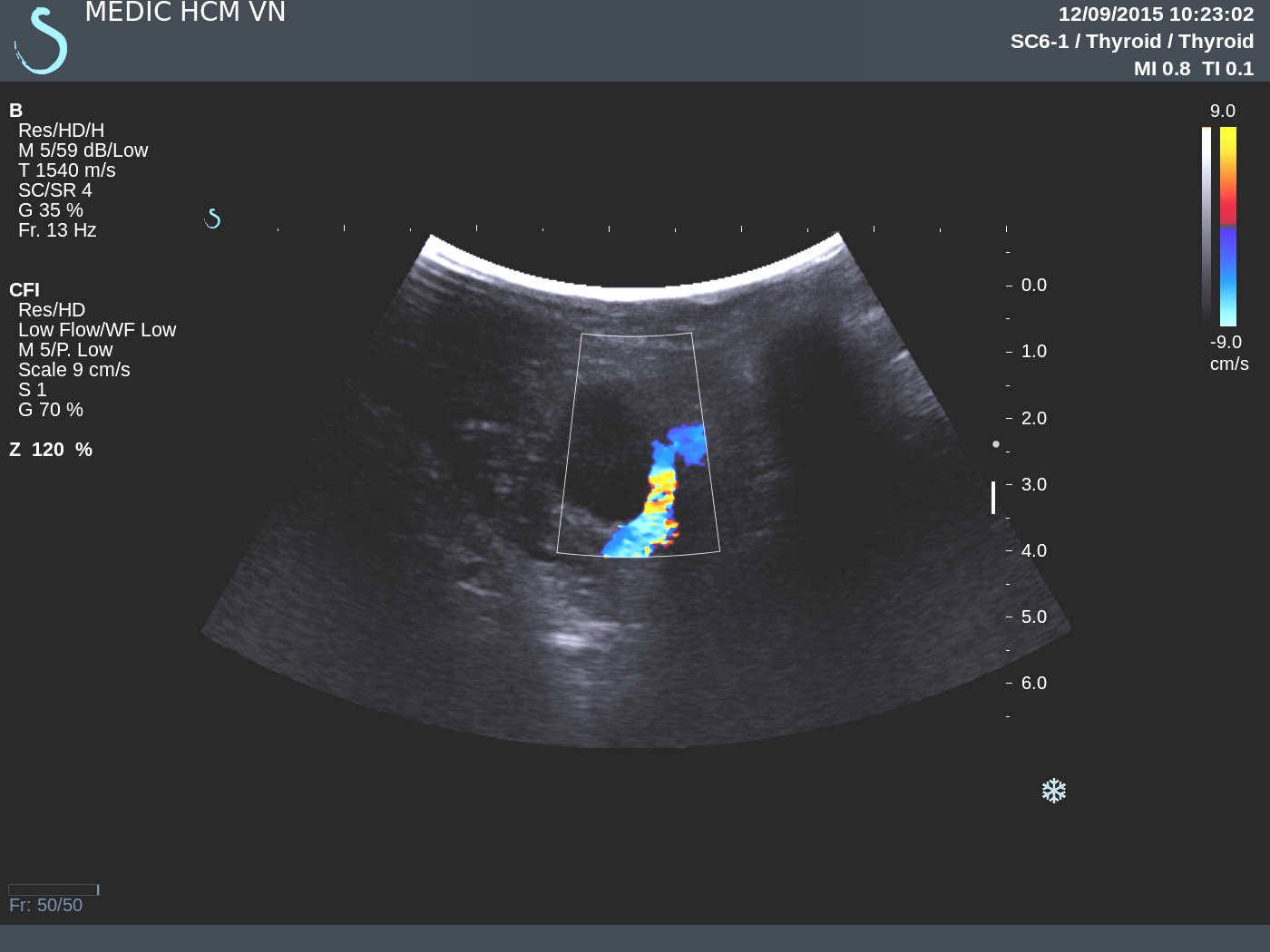
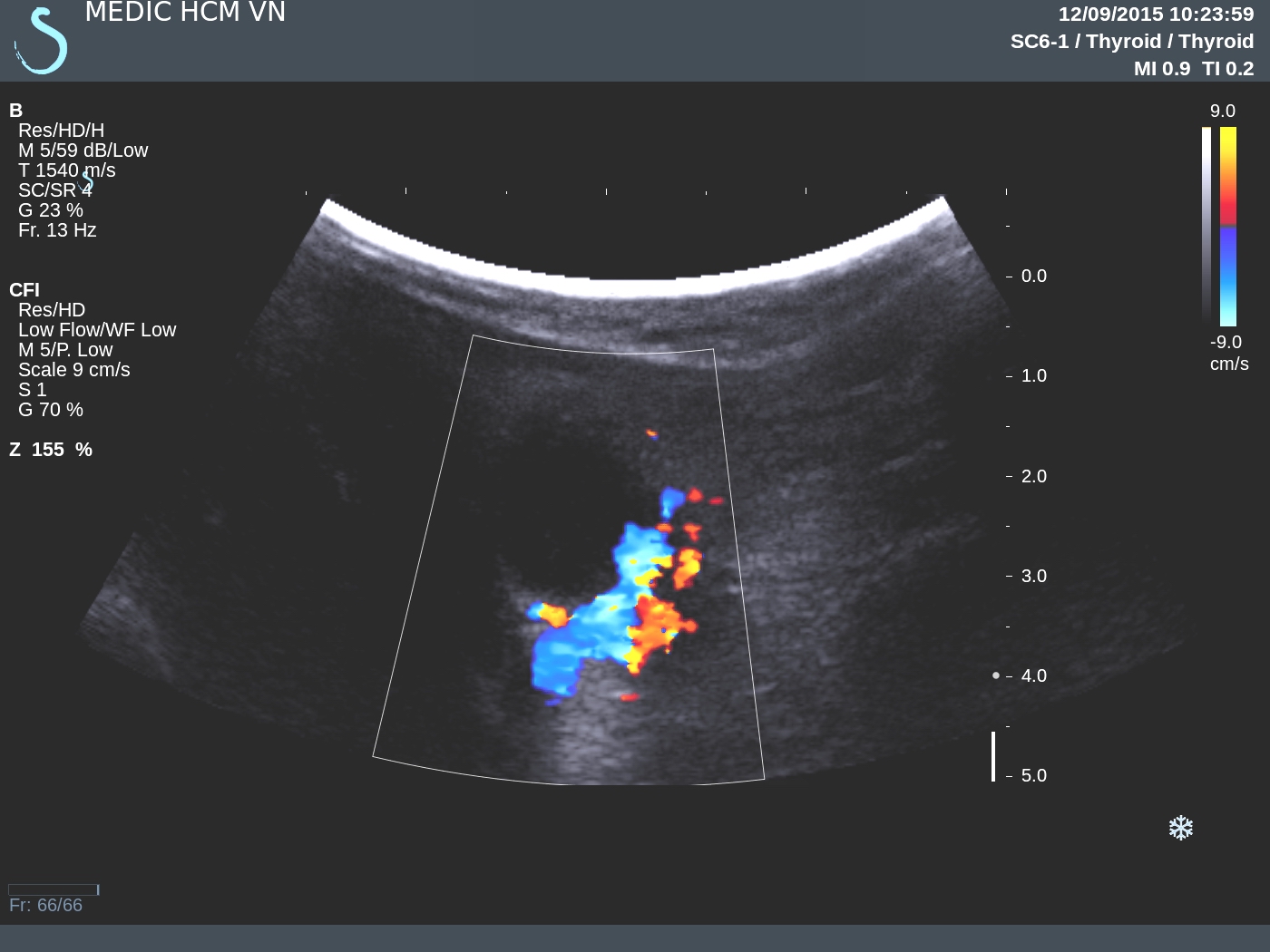
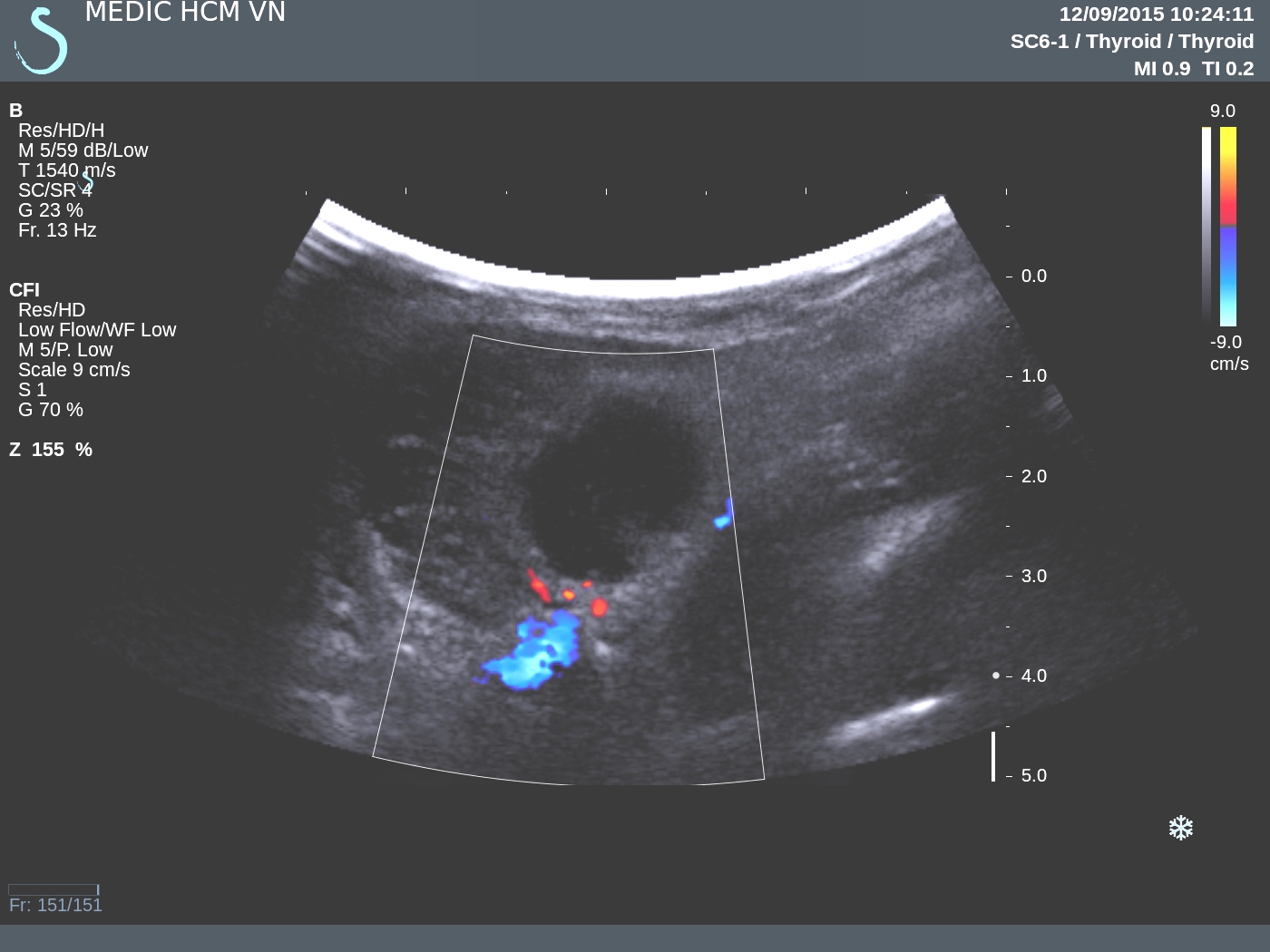
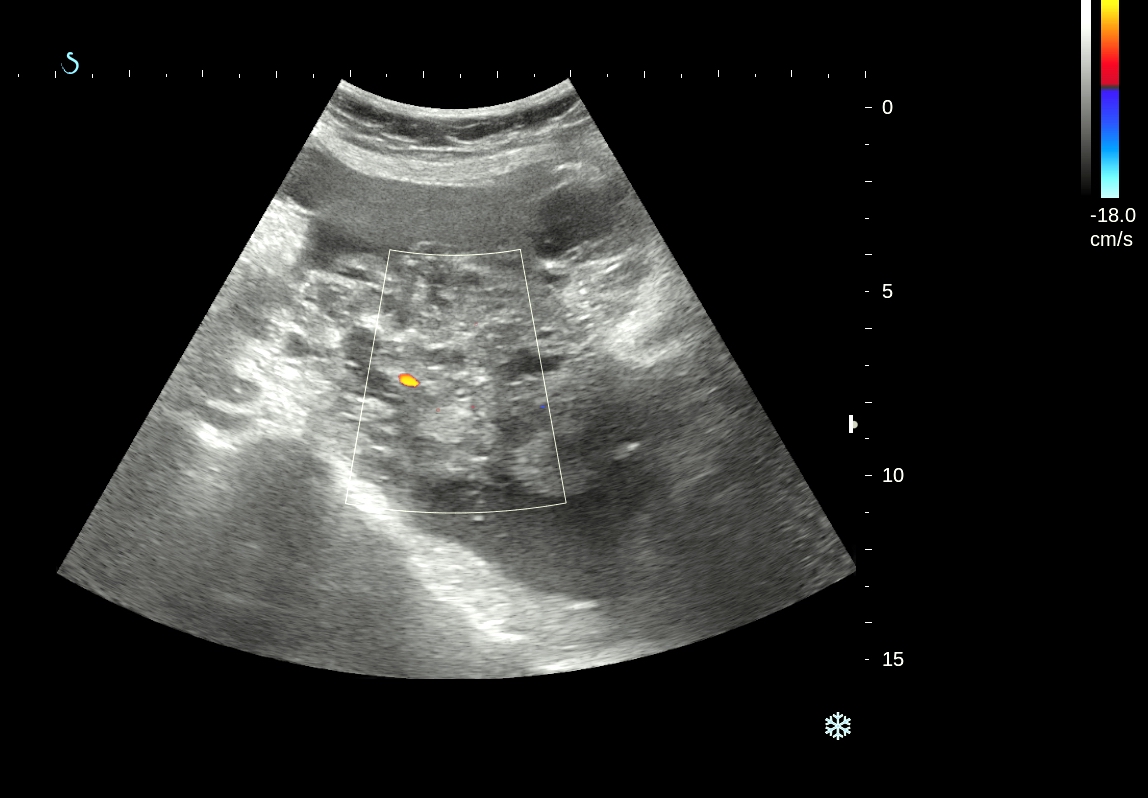
CASE 330 : SMALL HCC, Dr PHAN THANH HẢI, MEDIC MEDICAL CENTER, HCMC, VIETNAM
Man
66 yo with history no infected HBV, HCV but high values of liver enzymes for a long time.
Ultrasound of liver showed fatty
infiltrating in liver.
Blood test of HCC
RISK positive with AFP: 33.6 ng/ml; AFP-L3%: 62,4% and
DCP: 21mAU/mL.
MRI of liver with
PRIMOVIST and DWI detected a small focal lesion, size of 0.8cm at the liver border in
segment 6, very bright
in DWI and captured and washed out Primovist like a HCC.
Diagnosis was made for a small HCC, wait for operation.
DISCUSSION:
Biopsy or not for the case: hepatologist and radiologist said no because worrying of sedding cancer cells.
MayoClinics Report HCC_AFP_L3
DISCUSSION:
Biopsy or not for the case: hepatologist and radiologist said no because worrying of sedding cancer cells.
RFA or SURGERY? RFA could perform if ultrasound can see the tumor. Yes, WE CAN SEE THIS HCC ( see 2 US pictures).
This case is planning to do RFA in next week and test HCC Risk (WAKO) 24 hours after this procedure.
After 48 hrs RFA [ 27-08-2015] 2nd Wako test repeated (AFP: 21.7 ng/ml, AFP-L3 : 60.5%, DCP: 21mAU/mL
Wako test again 10 days after RFA [ 6-09-2015] 3rd Wako test ( AFP: 7.6ng/ml, AFP-L3: 42.1%,DCP: 20 mAU/mL)
Wako test will be performed one month after RFA.
REFERENCE:Wako test again 10 days after RFA [ 6-09-2015] 3rd Wako test ( AFP: 7.6ng/ml, AFP-L3: 42.1%,DCP: 20 mAU/mL)
Wako test will be performed one month after RFA.
MayoClinics Report HCC_AFP_L3
Subscribe to:
Posts
(
Atom
)