XIN DOWNLOAD THEO LINK ĐỂ THẤY HÌNH
FOR PICTURES PLS DOWNLOAD LINK BELOW.
MAN 83
YO HAD BEEN TREATED LUNG CANCER WITH CHEMOTHERAPY AND
RADIATION FOR 2 YEARS.
ONE MONTH AGO HE DETECTED SMALL SKIN
TUMOR AT LEFT TEMPORAL SCALP RAPID GROWING AND BLEEDING ( SEE
PICTURE).
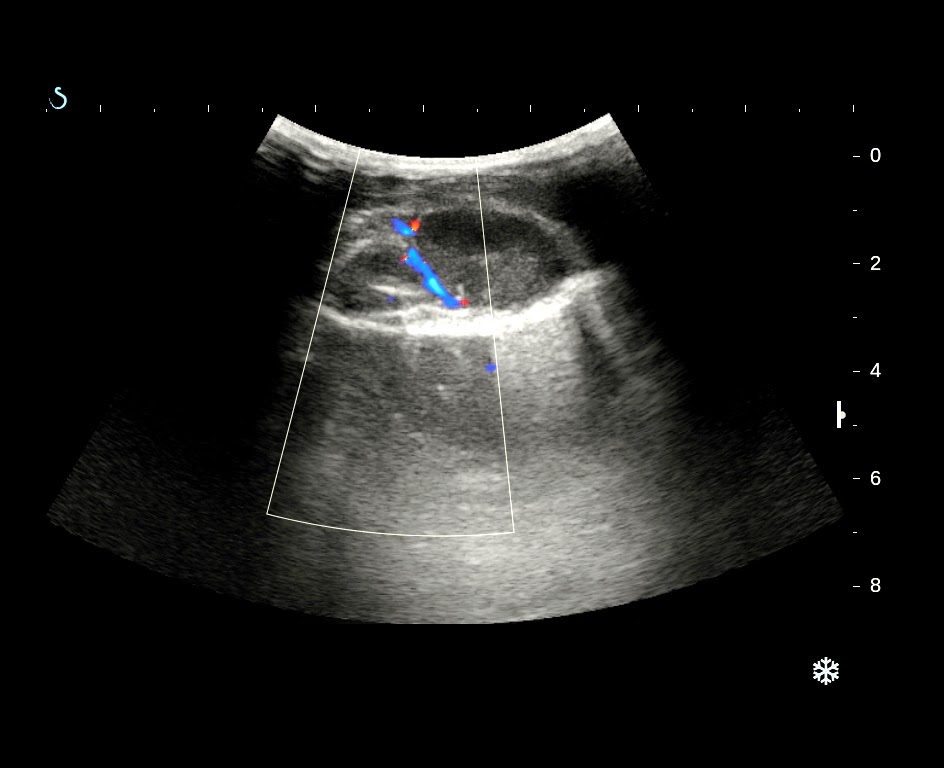
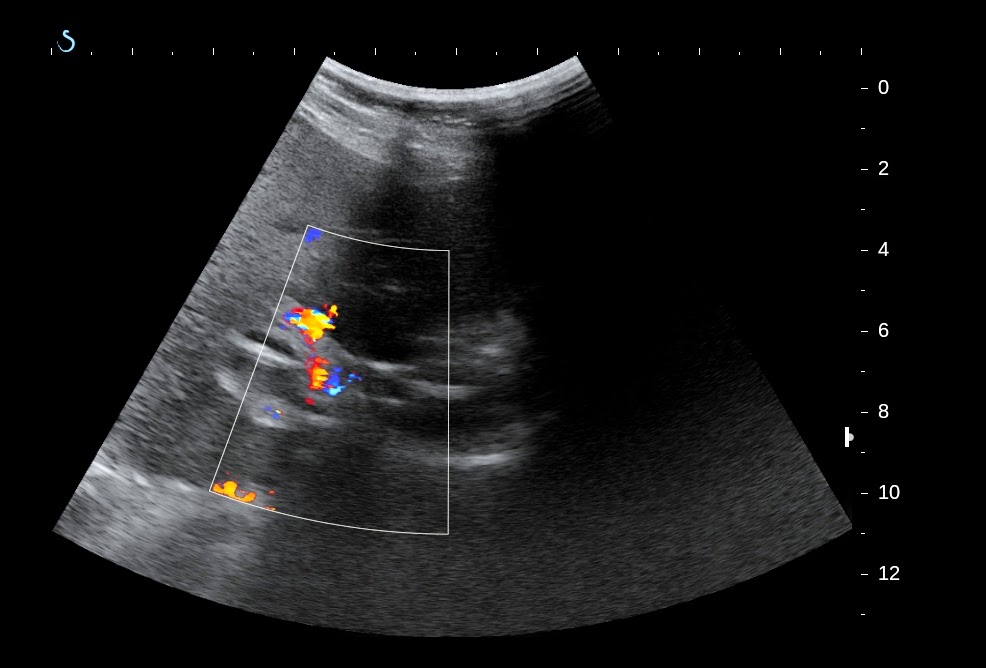
ULTRASOUND SCAN REPORTED THIS TUMOR BEING FROM THE SCALP NO INVADE TO BONE ( SEE 2 US PICTURES) AND LIVER METASTASIS ( US PICTURE 3)
MSCT CONFIRMED THE SCALP TUMOR NOT ERODING THE BONE, MANY METASTATIC LESIONS FROM THE LUNG TUMOR TO BOTH SIDE OF LUNG, LIVER, ADRENAL GLAND.
BIOPSY OF THIS TUMOR CONFIRMED THAT METASTASIS FROM LUNG CANCER, SQUAMOUS CELL CARCINOMA..
SUMMARY: LUNG CANCER SOMETIMES METASTASES TO SKIN OF SCALP AND NOT TO BONE.
REFERENCE: