A 56 yo male patient undergoes hoarse voice for 6 months after screaming, now out of breath talking loud voice.
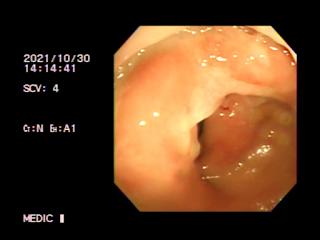
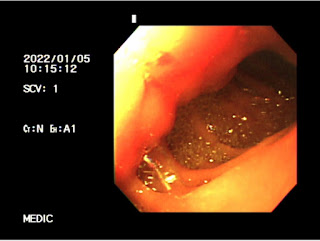
Laryngoscopy= Left apical arytenoid cartilage incompletely closed.
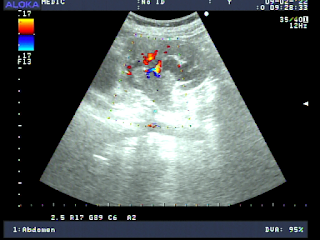
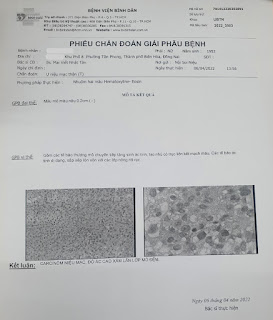
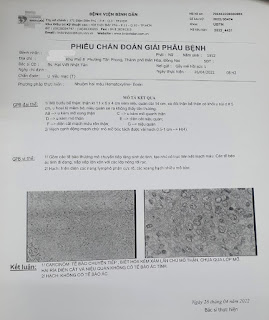
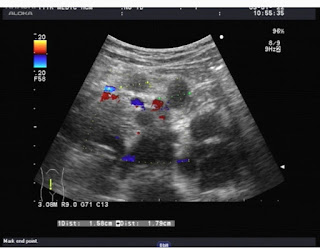
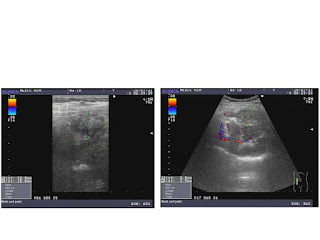
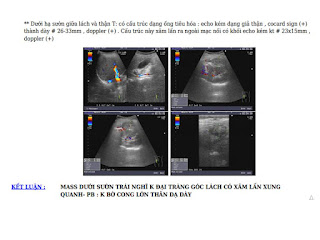
Cardiac ultrasound detected descending thoracic aneurysm witth aortic wall lesions.
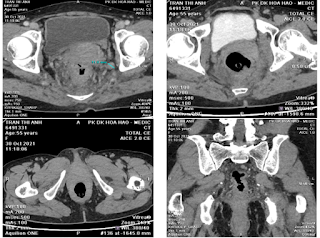
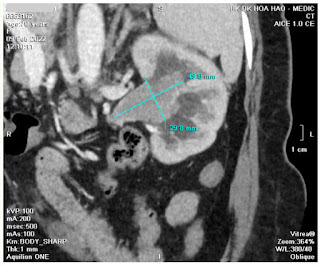
MSCT confirmed atresia of left vocal cord and descending thoracic aneurysm in saccular form, non dissecting.
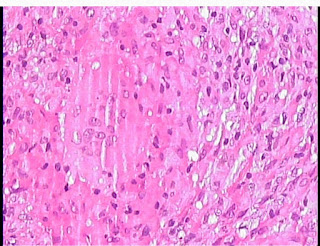
The recurrent laryngeal nerve RLN *from vagus nerve * supplies muscles of the larynx with the posterior and lateral cricoarytenoid.

In the case, descending thoracic aneurysm with aortic wall lesions may damaged the left RLN nearby which makes him the hoarse voice.